Reasons for Low Hearing Loss Treatment
Key Takeaways
- Only 16% of people between the ages of 20 and 69 who need hearing aids actually use them.
- Hearing aids are the third-largest material purchase for many people, behind a house and a car.
- Roughly 28.8 million U.S. adults could benefit from hearing aids.
- Barriers such as high cost, stigma, lack of accessibility, and poor customer satisfaction have traditionally kept people from buying hearing aids.
- Hearing aids can improve quality of life, help ease depression, and decrease the risk of dementia and falls
Hearing loss is a common condition in older adults, affecting 68% of Americans in their 70s and 90% in their 80s and older.5 It not only limits a person’s ability to communicate, but also increases the risk of significant health conditions, like dementia, depression, and anxiety.6
Given the importance of hearing health and the fact hearing loss is becoming more prevalent due to an aging U.S. population,7 it’s surprising that among adults age 20–69 who need hearing aids, only one in six use them.3 With a high incidence of hearing loss and the associated health risks, why aren’t more Americans seeking treatment?
Our team wanted to find out more, so we investigated national data, held focus groups, and talked to hearing care experts, device manufacturers, and people with hearing loss (both those who wear hearing aids and those who don’t).
We learned that a number of obstacles keep people from buying hearing aids and using them consistently. But recent advancements in hearing aid design and technology, research findings on the impact of hearing ability on overall health, and legislation aimed at making hearing devices more affordable could add up to treatment that’s more accessible and attractive to the millions of Americans who need it.
How many Americans with hearing loss currently use hearing aids?
About 28.8 million American adults need hearing aids, but only 16% of people between the ages of 20 and 69 who need hearing aids use them, according to 2021 research from the National Institute for Deafness and Other Communication Disorders.3
And only 7.1% of adults over the age of 45 had used a hearing aid in 2019, with men using them more often than women, according to the National Health Information Survey. Adults 65 and older were also seven times as likely to have used hearing aids than adults in the 45–65 year age range.8
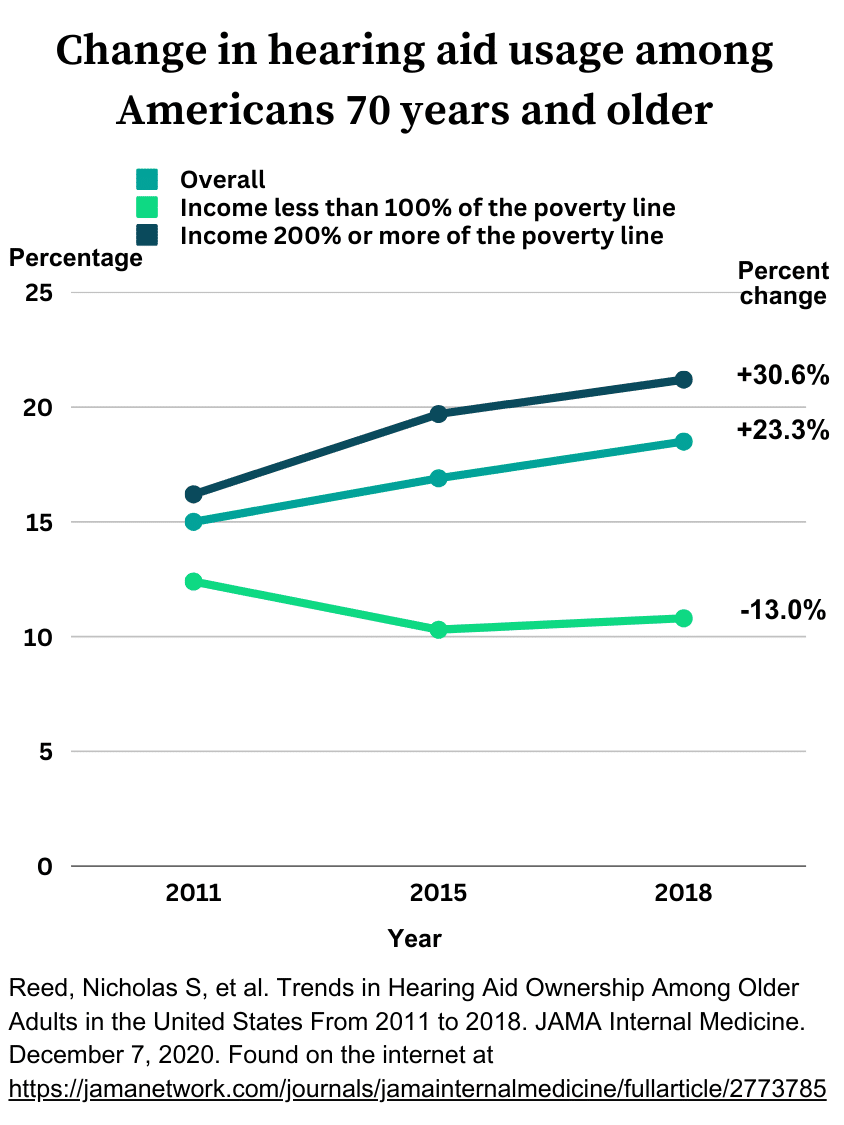
Data on hearing aid use in older adults is encouraging: more people 70 years and older are using hearing aids now than in years past, according to a study of hearing aid use among Medicare beneficiaries.9 From 2011 to 2018, there was a 23.3% increase in the number of people in this age group who used hearing aids, with one big caveat: Income level had a major impact. Only people living above the poverty line increased their use of hearing aids over the seven-year period.
Those with an income below the federal poverty line showed a downward trend in hearing aid use. This discrepancy is likely due to a number of factors, which may include the high cost of hearing aids, lack of insurance coverage for hearing exams and devices, and limited access to hearing health care.
Even with increases in certain segments of the population, hearing aid use in America continues to be low across the board. Hearing experts say a number of reasons are to blame.
Barriers to hearing aid use
What keeps people from getting their hearing loss treated? In contrast to vision problems, which are readily addressed with glasses or contacts (statistics show 75% of American adults use some form of vision correction),10 hearing aid use in America is surprisingly low. We set out to discover why, and here’s what we found.
#1 We underestimate the importance of hearing health
One of the most prevalent factors in delayed hearing loss treatment: Many people simply don’t think hearing loss is an important health condition to address.
Just as vision problems can hinder your quality of life and even your physical safety, hearing loss can be quite debilitating. Since both vision and hearing are part of the five senses, it’s vital to keep them functioning at optimal levels for cognitive health and overall wellness.11
But hearing loss is a condition that often comes on gradually with age, and many don’t take measures to treat it until they notice a significant impact on their daily lives. Statistics show most people wait an average of 10 years to get hearing aids after realizing they have hearing loss.12
Jennifer (who asked to only use her first name) is a 45-year-old physical therapist from Cincinnati, Ohio. She first noticed a problem with her hearing when her 12-year-old son began wearing hearing aids. “When I put his hearing aids on, I realize how much better I can hear everything around me,” she said.
When we asked Jennifer if she would consider getting hearing aids for herself, she said she wasn’t ready yet, noting they might make her feel old, she wouldn’t want other people to notice them, and she didn’t feel her hearing loss was interfering with her day-to-day activities yet. But while Jennifer was surprised to learn hearing loss plays a key role in maintaining cognitive health, she still didn’t feel she needed hearing aids right now.

Untreated hearing loss can raise your risk of a number of other health conditions.
Studies show hearing loss is linked to:6
- Dementia and other types of cognitive decline
- Communication problems
- Falls
- Social isolation
- Depression, anxiety, and other mental health issues
Because hearing loss is a common condition that affects the majority of older adults and often comes on gradually, it may seem like a normal part of aging that doesn’t need to be addressed. But 75% of Americans don’t realize hearing loss can raise the risk of the above health conditions, according to a 2022 survey of 1,250 adults.13
When you have hearing impairment, fewer sound signals make it to the brain for processing. As a result, nerve pathways normally used to interpret sound begin to process input from other senses, such as sight.14 The brain also has to work harder to decipher and assign significance to the sound signals it does receive.
The combination of decreased sound and increased cognitive load can add up to fatigue15 and impaired brain function,16 compounding the difficulties people already have with their hearing.
Hearing loss and dementia
The link between hearing impairment and dementia is an important one. The CDC reports that “in the United States, 6.2 million people age 65 and older have Alzheimer’s disease, the most common type of dementia.” Up to 40% of dementia cases could be delayed or prevented by addressing contributing factors such as hearing loss.17
While overall rates of dementia have been declining slightly in the U.S., states with higher numbers of older adults are predicted to see an increase in Alzheimer’s disease over the next few years.18
What could make someone more likely to get their hearing loss treated? One review published in 2023 revealed people with more severe hearing loss (both self-reported and determined by hearing tests), those who understand the functions and benefits of hearing aids, and those who view hearing aids positively are more likely to seek hearing loss treatment.19
#2 We’re not getting our hearing tested
The majority of people we talked to in personal interviews and focus groups didn’t know how to get their hearing tested or where to buy hearing aids.
In fact, older adults are more likely to get a physical or eye exam, have their cholesterol checked, or take their pet to the vet than they are to have their hearing evaluated, according to a 2022 survey.13

This is understandable, considering hearing checks are far from being a standard part of physical exams. Even when they are included, we found people aren’t always given recommendations for further testing if hearing loss is detected. The 2022 survey referenced above found only 23% of respondents had received a hearing test within the past year.13
Several of the audiologists we’ve talked to have shared that this is a shortcoming within their profession, and they see a need for better education on the significance of hearing health.
We spoke with Margaret Wallhagen, RN, PhD, FAAN, a professor at the University of California San Francisco with a research focus on hearing loss and access to hearing health care. “It’s important for people to begin using hearing aids when they have mild hearing loss rather than waiting until it’s more severe,” Wallhagen noted. But national data show use of hearing aids among people with mild hearing loss is extremely low, at just 4%.20
For an in-person hearing exam, visit a hearing care clinic staffed with an audiologist or hearing instrument specialist. Both of these types of hearing professionals can conduct a physical exam of your ear along with an audiometry exam to test your hearing with different sound frequencies, as well as your ability to hear and understand speech in the presence of background noise.21
You can also check your hearing online or with a smartphone app at no cost by searching for “free online hearing screening” or downloading a hearing screening app, such as Mimi. The Mimi app is convenient to use, and it gives you your Hearing Number, which is a measure of your overall hearing ability.
It’s important to note that audiology exams are covered by Medicare. Medicare covers a visit to an audiologist without a referral from a physician if the hearing loss or balance issue has existed for 12 or more months. For these qualifying patients, Medicare will cover the audiology visit once every 12 or more months.
#3 Hearing aids are expensive
The average cost of prescription hearing aids is $4,600 per pair.22 In many cases, that includes several years of follow-up care and maintenance. But it’s still more than many Americans can afford. According to recent research, hearing aids are the third-largest material purchase for many people, behind a house and a car.23 While hearing aids are an investment, they can last five to seven years with proper maintenance.
A 2018 survey of more than 10 million adults with hearing loss found up to 74% of Americans couldn’t afford hearing aids priced at $2,500 per pair, while 17% couldn’t afford a $500 pair of OTC hearing aids.24 With many prescription devices carrying a price tag $2,000 more than the average price used in this study, the vast majority of Americans who need hearing aids may not be able to pay for them.
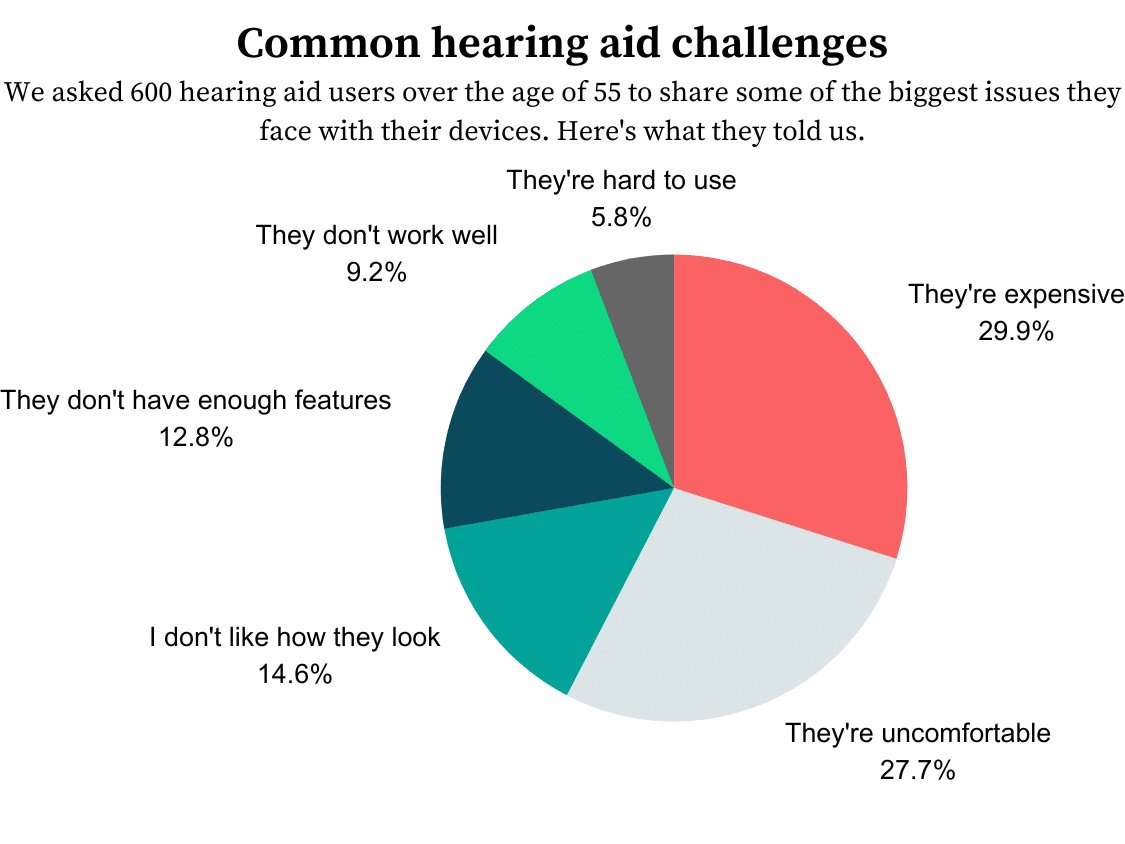
This cost obstacle was a common theme in our focus groups and interviews with people with untreated hearing loss. Our survey of 600 hearing aid users found 30% of respondents cited cost as their biggest obstacle to purchasing hearing aids.25
Unfortunately, Medicare and many private health insurers don’t provide much assistance. Medicare Parts A and B don’t provide coverage for hearing aids or hearing aid supplies, although Part B does cover hearing exams if ordered by a physician as part of a diagnosis.26
Medicare will cover a visit to an audiologist without a referral from a physician if the hearing loss or balance issue has existed for 12 or more months. For these qualifying patients, Medicare will cover the audiology visit once every 12 or more months.
Many private insurance companies don’t offer hearing benefits either, although some Medicare Advantage (Part C) and other private insurance plans do include coverage for hearing aids. But there’s no guarantee people who do have insurance coverage will use it to treat their hearing loss: Only 8% of Medicare beneficiaries use hearing health services, even if their plan includes hearing benefits.11
#4 Access to health care is limited
Hearing aids have traditionally required the services of a hearing care professional to conduct a hearing exam, dispense hearing aids, and program them to each person’s hearing loss profile. This can be a significant barrier for people who don’t live near a hearing care clinic.
One study found Americans living in rural areas wait longer to get their hearing loss treated and have to drive twice as far to obtain hearing care services compared to people in urban locations.27
Partly to address this concern, the FDA passed a final rule in October 2022 introducing OTC hearing aids to the American public, making the United States the first country to allow the sale of hearing aids without the involvement of a hearing professional.28
OTC hearing aids are appropriate for adults 18 and older with perceived mild to moderate hearing loss. We’ve found the average price is around $1,600 per pair, although it varies quite a bit depending on features and technology. But OTC hearing aids typically don’t come with the same level of support you’ll find with prescription hearing aids bought at a hearing care clinic. And some adults may need more expensive prescription hearing aids due to more severe hearing loss and the need for in-person support. Still, the remote care offered by most OTC hearing aid companies opens a much-needed path to hearing care access for those who don’t live within driving distance of a hearing clinic.
A few OTC hearing aid companies, including Eargo and MDHearing, are working with private insurers to cover hearing aids. And a bill to include hearing benefits in Medicare was reintroduced this year by Rep. Debbie Dingell, D-Mich., and Rep. Brian Fitzpatrick, R-Penn. We’ll be watching closely to see if and when insurance coverage for hearing aids improves.
#5 We have high expectations
When you pay thousands of dollars for hearing aids, it’s understandable to expect a lot regarding performance, comfort, and fit. Wallhagen put it into perspective. “If I pay a lot of money for a computer, I’m going to expect it to do a lot for me, and to work well,” she said.
“If I pay a lot for a hearing aid, I expect it to work, and so if I don’t see the cost-benefit ratio as valuable, I’m probably not going to be very pleased with it. [But] it’s important to keep in mind hearing aids are aids and do not cure hearing loss or correct the underlying damage to the inner ear,” she noted.
It’s understandable to hope hearing aids will completely restore hearing ability. That doesn’t always happen. Recent research shows the longer hearing loss goes untreated, the more severe it often becomes and the harder it can be to treat.29 Audiologists we’ve spoken with say the earlier they can diagnose and treat hearing loss, the better a person’s chances to improve their hearing ability and enjoy long-term success with hearing aids.30
During our discussions with a focus group of people with hearing loss, we asked them what they were looking for in hearing aids and got the following responses:
- “They should be comfortable to wear.”
- “I’d like to have hearing aids with good sound quality.”
- “Hearing aid batteries need to be easy to change, and rechargeable hearing aids would be even better.”
High expectations coupled with a lack of knowledge about how to achieve success can lead to disappointment. A review of hearing aid market research showed varying degrees of customer satisfaction with hearing aids, ranging from 50%–91%.31 Consumers want comfort, convenience, and high performance in their hearing aids, but the reality can be quite different.
Here are some of the most prevalent challenges encountered by hearing aid users, according to our survey of older adults who own hearing aids.
On a performance level, our focus group of hearing aid users reported their devices tended not to meet their expectations in the following areas:
- Sound clarity
- Difficulty localizing sounds in noisy environments
- Getting used to how they feel in the ear
- Understanding conversations
The last point is a challenge we’ve heard repeatedly from consumers—a hearing aid user in our focus group shared her frustrations with the continued difficulty she has understanding conversations, even while wearing her hearing aids. “I still have to ask people to repeat themselves. A lot of times I just blow them off and accept I can’t understand what they said,” she said.
For success with hearing aids, consistency is key
We uncovered yet another telling gap between consumer expectations and what hearing care professionals say is necessary for long-term success with hearing aids. Many people expect hearing aids to work like earbuds or eyeglasses: Put them in when you need them, and take them out when you don’t.
But the goal of wearing hearing aids is more complex. In contrast to devices that allow you to listen to music or see more clearly in certain situations, hearing aids are designed to help you hear better in every environment and enable your ears and brain to take in and process more sound than they have in the past.
With consistent use, hearing aids may improve cognitive health and increase the activity of sound-processing pathways in the brain.32 But what many consumers aren’t aware of: To reap the full benefits of hearing aids, you must wear them consistently, for as long as possible each day.
Hearing experts at the Cleveland Clinic advised new hearing aid wearers to put on their hearing aids when they wake up in the morning and keep them in all day long.33 The only time you should take them out is when there’s a risk of them getting wet, such as when you go swimming, take a shower, or use hairspray or other hair products.
Multiple hearing aid users we talked to wear their hearing aids only occasionally, often when they’re going somewhere noisy (like a restaurant) and they know they’ll need extra help understanding conversations. But this isn’t the best strategy, because your brain needs to take in and process more sounds all the time to rebuild pathways that may have been lost when your hearing loss was untreated. According to the authors of a 2021 review on hearing aids and cognition, “Wearing a device regularly and often is the only means to ensure the brain has had the ability to adapt to increased auditory stimuli.”34
If you’re not happy with your hearing aids, follow up with your audiologist or hearing instrument specialist to make sure the physical fit of your hearing aids is correct. Your hearing professional can make sure they’re comfortable, help you learn what to expect with your new hearing aids, show you how to keep them clean and in working order, reprogram them if needed, and explain the importance of wearing your hearing aids consistently, even when you’re at home or in a quiet environment.
According to Nicholas Reed, an audiologist at Johns Hopkins University in Baltimore, Maryland, you can think of audiologists as counselors to their clients.
Can hearing aids really change your life?
Aside from the health effects of hearing loss, the impact hearing loss has on your daily life can range from a mild inconvenience to a severe impediment to your work, daily activities, and enjoyment of relationships.
While even the best hearing aids can’t completely restore hearing, they can greatly improve it and enhance your quality of life. Jacquelyn Lovitt, AuD, from the Capital Institute of Hearing and Balance in Baltimore, Maryland, shared with us how hearing aids have impacted her patients’ lives.
The bottom line: Hearing aid use, while far from being commonplace in America, may become more of a reality for many people, thanks to lower-priced OTC hearing aids and newer technology aimed at making them easy to use with higher performance than hearing aids of the past.
As new manufacturers continue to enter the space, hearing care professionals and companies develop new ways to serve their customers, and legislators negotiate public health coverage of hearing aids and services, the market will be a changing landscape for some time to come.
Have questions about this article? Email us at reviewsteam@ncoa.org.
-
Livingston Gill, et al. Dementia Prevention, Intervention, and Care: 2020 Report of the Lancet Commission. The Lancet. July 30, 2020.
-
Centers for Disease Control and Prevention. Public Health and Scientific Information. December 11, 2018.
-
National Institute on Deafness and Other Communication Disorders. Quick Statistics About Hearing Loss. March 25, 2021.
-
Grandview Research. Hearing Aids Market Size, Share, And Trend Analysis Report By Product Type, By Technology Type (Digital, Analog), By Type of Hearing Loss, By Patient Type, By Sales Channel, By Region, And Segment Forecasts, 2023 – 2030.
-
Goman, Adele M. and Lin, Frank R. Prevalence of Hearing Loss by Severity in the United States. American Journal of Public Health. 2016.
-
Nieman, Carrie L., et al. Racial/Ethnic and Socioeconomic Disparities in Hearing Health Care Among Older Americans. Journal of Aging Health. February 2016.
-
Goman, Adele M., et al. Addressing Estimated Hearing Loss in Adults in 2060. JAMA – Otolaryngology Head & Neck Surgery. July 2017.
-
Centers for Disease Control and Prevention. Hearing Difficulties Among Adults: United States, 2019. July 2021.
-
Reed, Nicholas S, et al. Trends in Hearing Aid Ownership Among Older Adults in the United States From 2011 to 2018. JAMA Internal Medicine. December 7, 2020.
-
The Vision Council. Organizational Overview. 2021.
-
Willink, Amber, et al. Dental, Vision, and Hearing Services: Access, Spending, and Coverage for Medicare Beneficiaries. Health Affairs. February 1, 2021.
-
Johns Hopkins University. The Hidden Risks of Hearing Loss.
-
Carlson, Matthew L, et al. Awareness, Perceptions, and Literacy Surrounding Hearing Loss and Hearing Rehabilitation Among the Adult Population in the United States. Otology & Neurotology. March 2022.
-
Campbell, Julia and Sharma, Anu. Cross-Modal Reorganization in Adults With Early Stage Hearing Loss. PLOS One. Feb. 28, 2014.
-
American Academy of Audiology. What Is Listening Fatigue?
-
Powell, Danielle S, et al. Hearing Loss and Cognition: What We Know and Where We Need to Go. Frontiers in Aging Science. Feb. 28, 2022.
-
Centers for Disease Control and Prevention. The Truth About Aging and Dementia. Sept. 8, 2021.
-
Weuve, Jennifer, et al. Prevalence of Alzheimer Disease in US States. Epidemiology. Jan. 2015.
-
Knoetze, Megan, et al. Factors Influencing Hearing Help-Seeking and Hearing Aid Uptake in Adults: A Systematic Review of the Past Decade. Trends in Hearing. Feb. 16, 2023.
-
Chien, Wade and Lin, Frank R. Prevalence of Hearing Aid Use Among Older Adults in the United States. Archives of Internal Medicine. Feb. 13, 2012.
-
Medline.gov. Audiometry.
-
National Academies of Sciences, Engineering, and Medicine. Hearing Health Care for Adults: Priorities for Improving Access and Affordability. 2016.
-
Lin, Frank R, and Chadha, Shelly. Over-the-Counter Hearing Aids—Using Regulatory Policy to Improve Public Health.
-
Jilla, Anna Marie and Johnson, Carole E. Population-Based Perspectives on the Affordability of Hearing Aids. The Hearing Journal. Dec. 2020.
-
NCOA Hearing Aids Survey. 600 respondents. Conducted using Pollfish. Launched March 2022.
-
Medicare.gov. Hearing Aids.
-
Chan, Stephen, et al. Rurality and Determinants of Hearing Healthcare in Adult Hearing Aid Recipients. The Laryngoscope. October 2017.
-
Federal Register. Medical Devices; Ear, Nose, and Throat Devices; Establishing Over-the-Counter Hearing Aids. Aug. 17, 2022.
-
National Institute on Aging. Hearing Loss: A Common Problem for Older Adults. Jan. 19, 2023.
-
American Speech-Language-Hearing Association. Untreated Hearing Loss in Adults. Jan. 2012.
-
Wong, Lena LN, et al. Hearing Aid Satisfaction: What Does Research From the Past Twenty Years Say? Trends in Amplification.
-
Cleveland Clinic. 6 Tips for Getting Used to Your New Hearing Aids. July 21, 2022.
-
Jiang, Fan, et al. Association Between Hearing Aid Use and All-Cause and Cause-Specific Dementia: An Analysis of the UK Biobank Cohort. The Lancet Public Health. May 2023.
-
Sarant, Julia, et al. The Effect of Hearing Aid Use on Cognition in Older Adults: Can We Delay Decline or Even Improve Cognitive Function?Journal of Clinical Medicine. 2020. Jan. 17, 2020.
